
Weight Loss / Bariatric Surgery is the ONLY proven method for long term weight loss when all other modalities fail. The team of experts spearheaded by Dr Raj Palaniappan employs several different bariatric surgical techniques and is one of the few in the world to perform all types of bariatric surgeries including all available techniques as well. Choosing the most appropriate method depends on various factors including body weight, various disease condition, nutritional status and your lifestyle. This high volume bariatric center has an enviable recored with regards to patient outcome and quality of life.
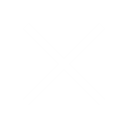
Laparoscopic Gastric Banding is one of the least invasive treatments where a band is placed horizontally around the upper part of the stomach. This involves incision of small abdominal cuts with minimal scarring and discomfort. Since the outlet is small, food stays in the pouch longer and one also feels satiated for a longer time. The small pouch ensures that the patient feels full after eating only small amounts of food.
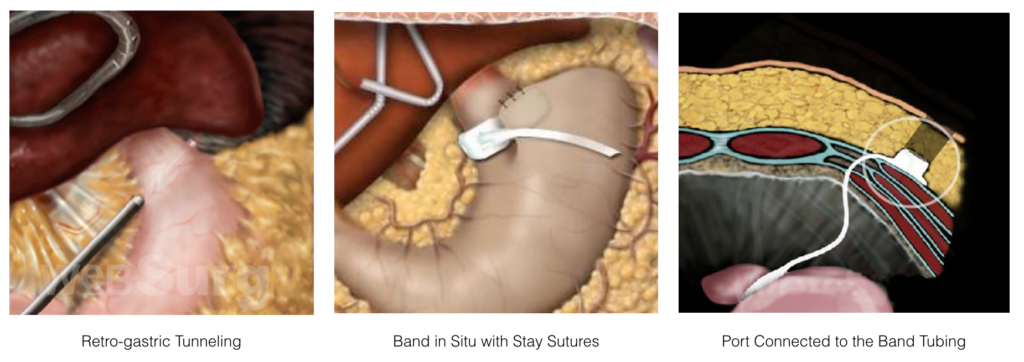
Laparoscopically, this involves making three to five small incisions in the abdomen to approximately remove 2/3rd of the left side of the stomach using Endoscopic staplers. This makes the stomach in the shape of a banana. The outlet valve and the nerves of the stomach remain intact, while only the size of the stomach is reduced. This not only decreases food intake to around 80 – 100 cc, it also increases the transit of food into the intestine and aids in the resolution of diseases.
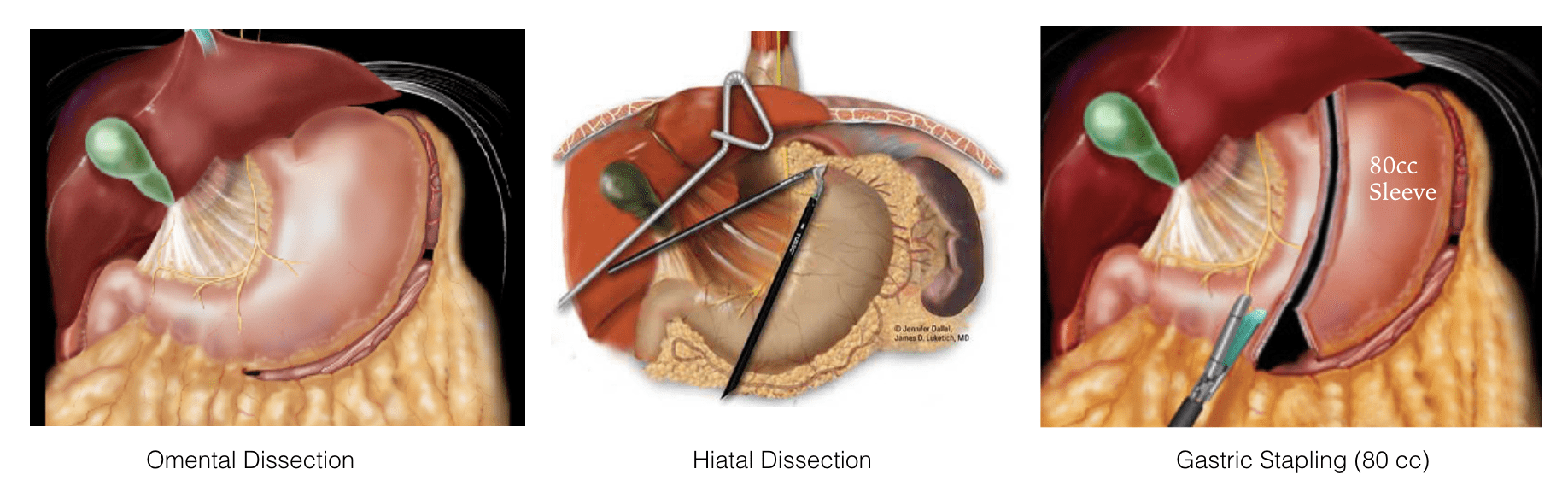
This involves the creation of a stomach pouch where the stomach is reduced to a small pouch of 25-30 cc volume and proximal small intestine (jejunum) is bypassed and connected to the new pouch for malabsorption. The stomach is literally reduced to the size of an egg, which aggressively reduces the amount of food intake and reduces the amount of fat and calories absorbed too. This procedure is now also performed with the addition of a band on the pouch for effective long term weight management.
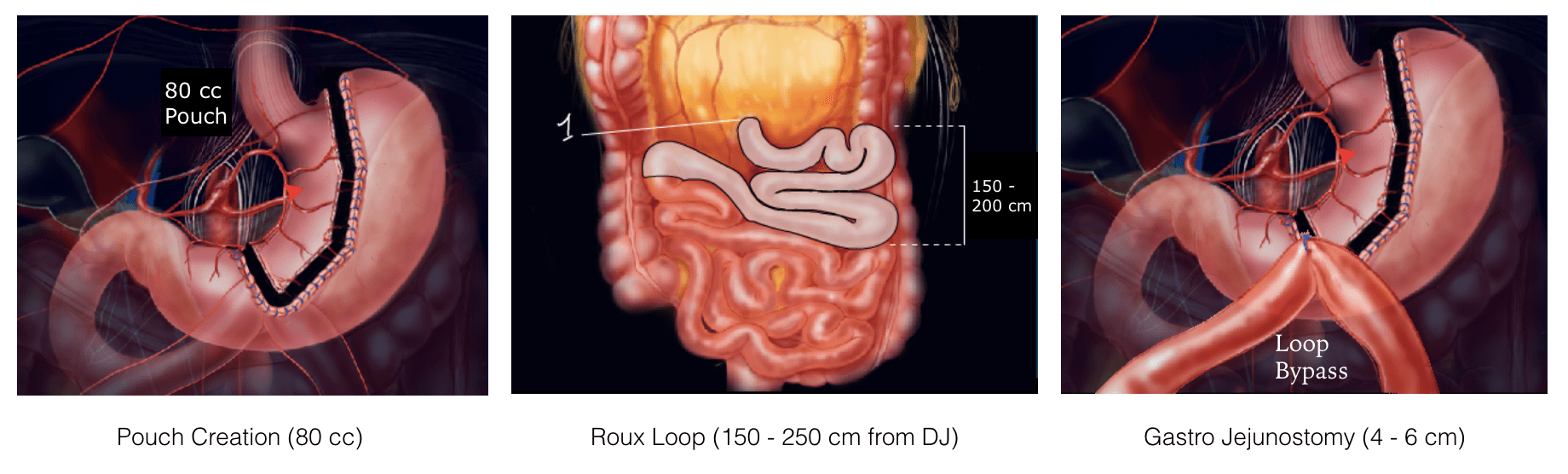
OAGB or Modified Mini Gastric Bypass (MGB) is a less complex and more Metabolic surgery than RYGB. Here the stomach pouch is made longer with a capacity of 60 – 80 cc and a loop of the proximal small intestine is chosen between 150 – 250 cm from the starting point and is anastomosed to the bottom of the stomach pouch. The procedure has gained immense popularity due to its powerful outcome despite being a less complex bypass procedure. However, it also is mired in controversies related to bile reflux. At present OAGB has the maximum rate of growth for any Bariatric procedure across the globe.
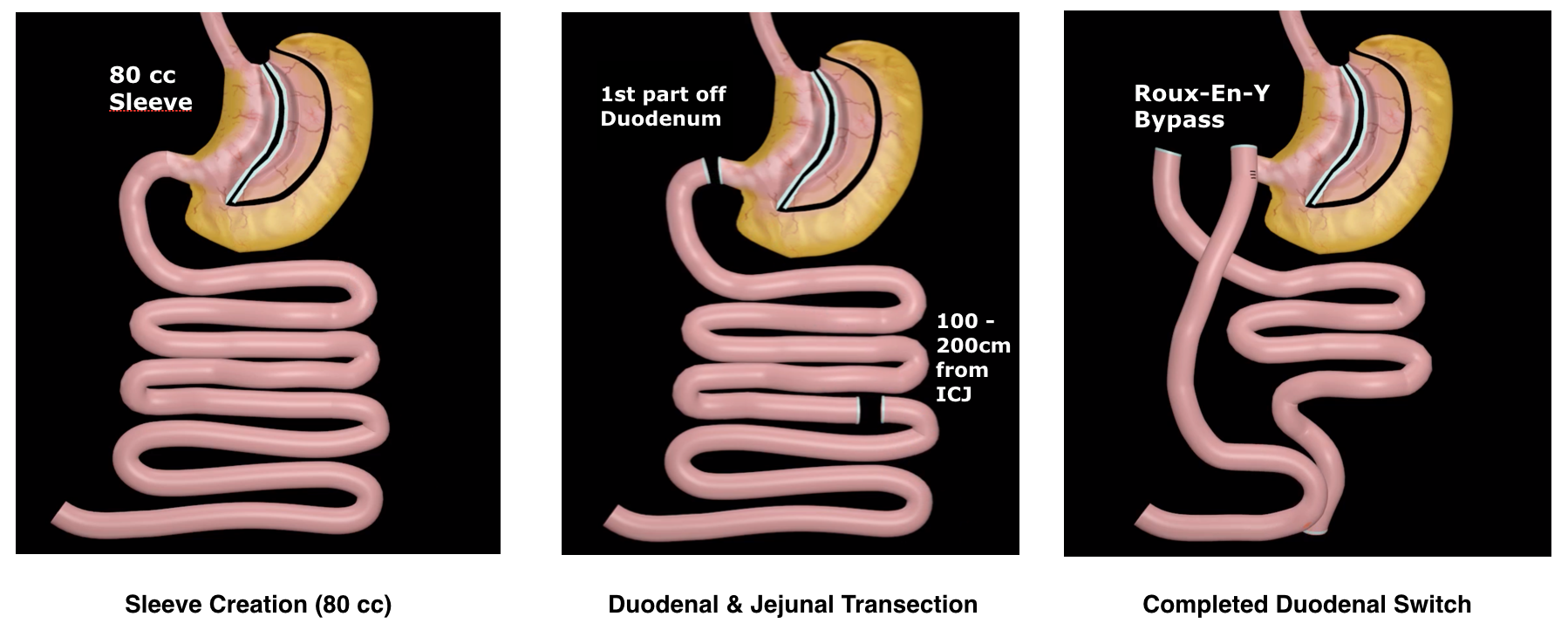
The treatment involves making a sleeve laparoscopically as the first part to give the benefit of a sleeve surgery. The power of surgery is doubled through bypassing the proximal part of the small intestine, just distal to the gastric outlet valve (duodenum) and reconnected into the distal small intestine (ileum) so, fewer calories are absorbed, appetite is reduced and this also strongly controls weight and disease process associated with obesity. Since this is considered a strong procedure, it is reserved for a select population.
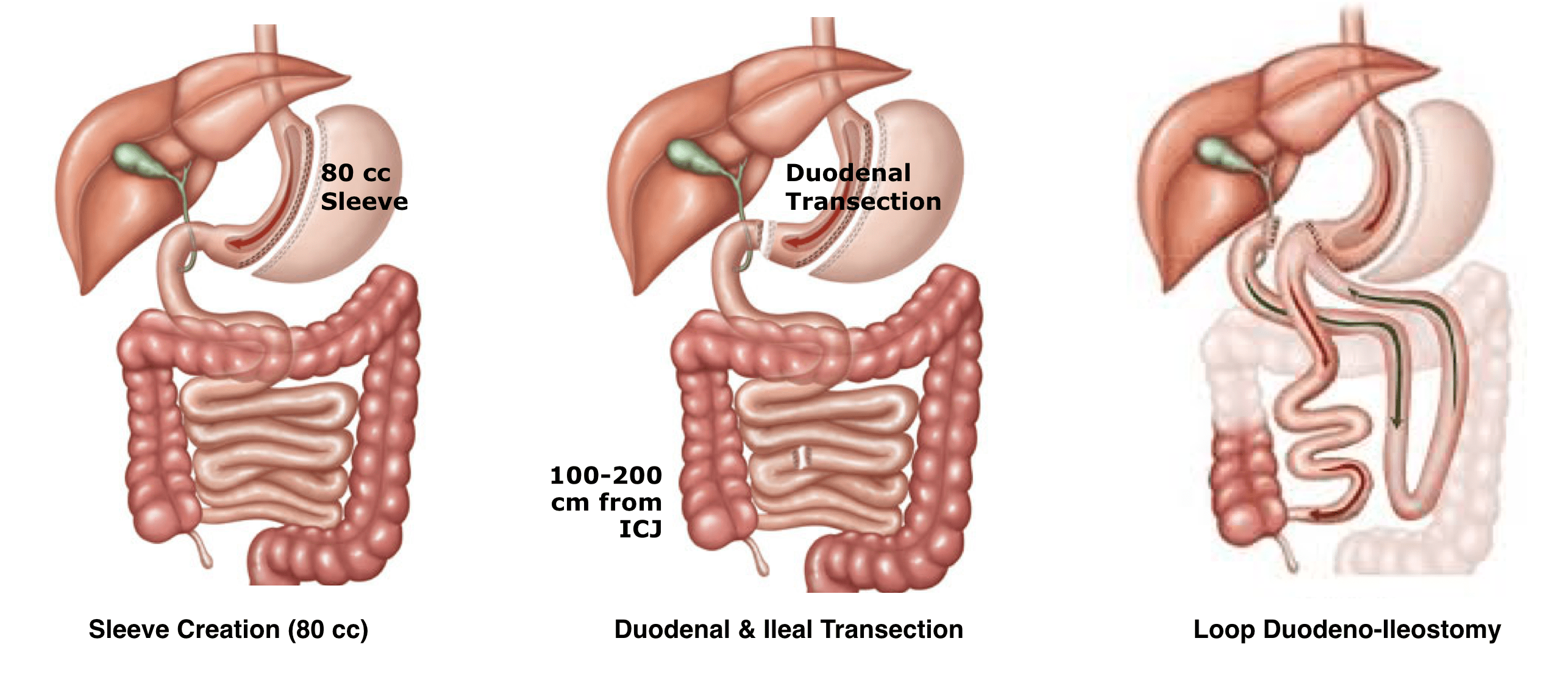
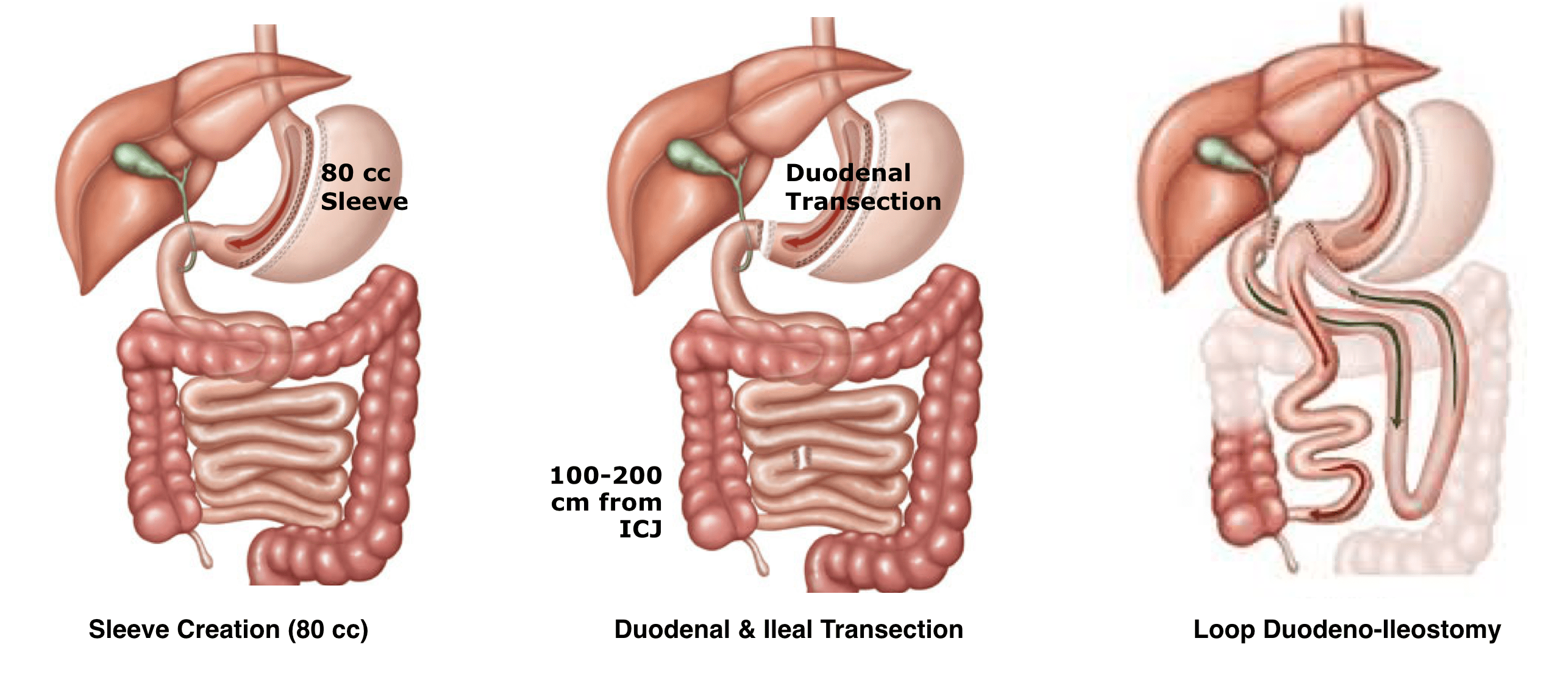
The objective of this surgical technique is to lessen the intestinal loop where nutrients are absorbed. A small gastric sleeve is created by sectioning the greater curvature of the stomach, as in the sleeve technique. Subsequently, the duodenum is transected beyond the pylorus. A duodenum-intestinal anastomosis is carried out 250 – 350 centimeters from the distal end of the small intestine (ileocecal valve). Therefore, the common channel where nutrients are absorbed becomes less which makes this a strong metabolic procedure.
SASI otherwise called as Transit Bipartition is a new addition to the list where a gastric sleeve is made together with gastric bypass by connecting a stomach exit with the intestine after bypassing proximal part of it. All this is done without separating the stomach exit and so, there will be two ways for passage of food: 30% of food passes in its normal passage and so vitamins and minerals are absorbed better. 70% of food passes in gastric bypass passway and so, a lot of food and sugars are not absorbed which results in weight loss and treatment of diabetes.
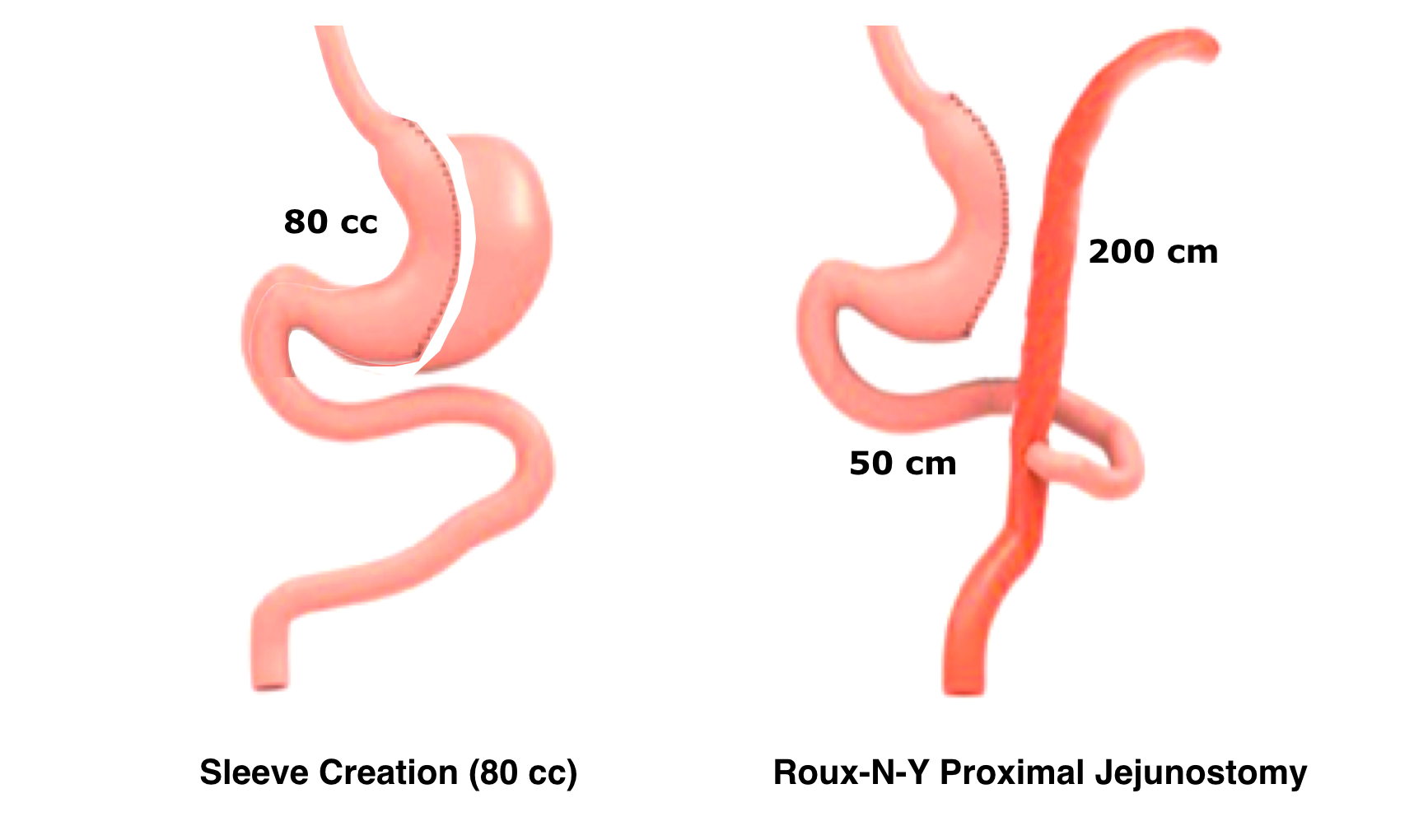
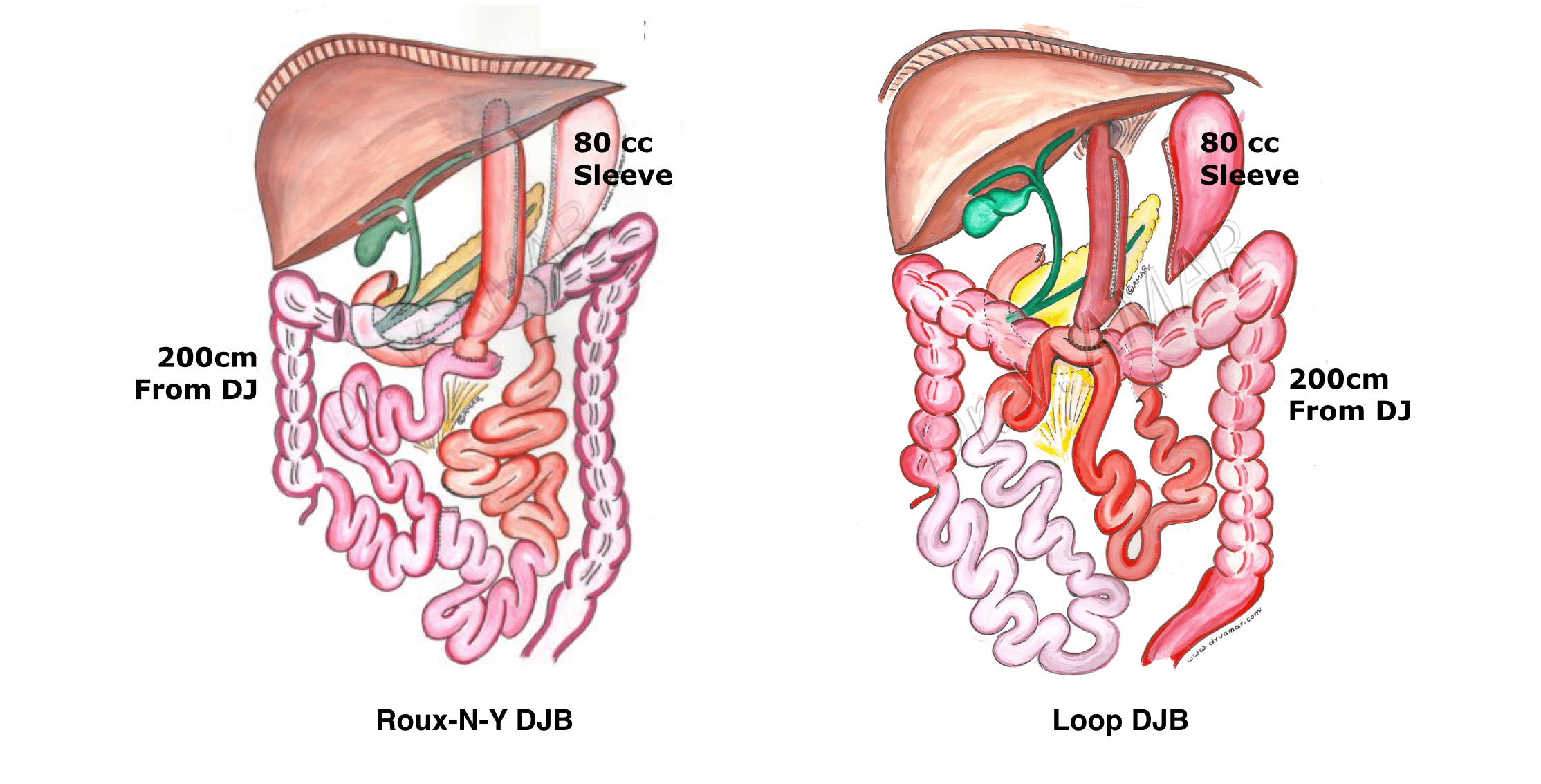
This involves the creation of a gastric sleeve of 80 -100 cc volume and proximal small intestine (150- 200 cm of jejunum) is bypassed and re-connected to the distal jejunum for malabsorption. The stomach is reduced like a hockey stick, which aggressively reduces the amount of food intake. The bypassed proximal small intestine will reduces the amount of calories and fat absorbed too.
It is a pylorus (lower stomach valve) preserving bypass where effectively a sleeve gastrectomy is performed as the first part of the procedure (see sleeve gastrectomy for details). Following this, the second step of small intestine anastomosis similar to RYGB or OAGB is prepared but is connected to the first part of the duodenum (small intestine). The sleeve part of the procedure can be tailor-made to suit the required weight loss of the patient, which makes it a safe surgery for non-morbidly obese diabetics as well as morbid patients. BAROS team is one of the few recognized center for this type of diabetic surgery.
Being an ever-evolving field of surgery, plenty of newer techniques are in the experimental phase and will be available for standard use from time to time.The novel procedures that are being experimented include Gastric Pacers, Aspire Assist Gastric aspiration therapy, etc.However, these procedures can be offered to people under the clinical trial basis.